Incontinence associated dermatitis: challenges and solutions
Sally Williams RGN, Community Tissue Viability Nurse, Plymouth Community Healthcare
Introduction
The term Moisture Associated Dermatitis describes the spectrum of damage that occurs when a patient’s skin is exposed for prolonged periods to sweat, urine, faeces and exudate. Incontinence Associated Dermatitis (IAD) is skin damage due to moisture on the skin from urine and/or faeces, and is traditionally considered as being a specific problem of continence care [1]. Incontinence Associated Dermatitis can be painful, and is commonly misclassified as pressure ulceration [2].
Appropriate diagnosis, prompt treatment and management and/or removal of the irritant source are crucial to long-term treatment.
Moisture Lesions
A moisture lesion is described as a ‘reactive responses of the skin to chronic exposure to urine and faecal matter, which could be observed as an inflammation and erythema with or without erosion. Typically there is loss of the epidermis and the skin appears macerated, red broken and painful [3].
They are further describes by the All Wales Tissue Viability Group [4] as:
‘…being caused by urine and/or faeces and perspiration which is in continuous contact with intact skin of the perineum, buttocks, groins, inner thighs, natal cleft, skin folds and where skin is in contact with skin... Moisture lesions cause superficial loss of epidermis and/or dermis, which may be preceded by areas of erythema on intact skin. They will usually cause pain. The skin will either be excoriated which presents as superficial broken skin which is red and dry, or macerated presenting as red and white, wet, soggy and shiny. The pattern of skin damage is uneven apart from on the natal cleft when the damage presents as a linear vertical split in the skin. In the case of ‘kissing’ lesions the damage usually presents on either side of a skin fold’.
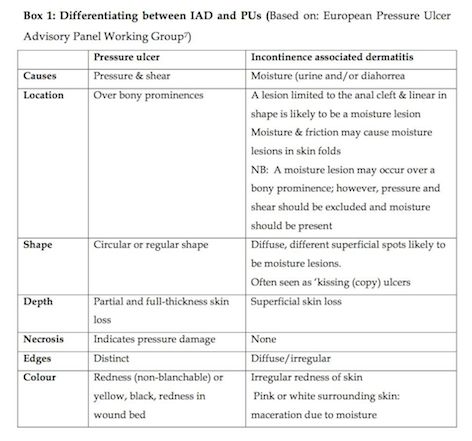
Skin affected by IAD has irregular, diffuse margins in the locations exposed to urine and faeces than pressure ulcers. In addition, IAD does not cause a full thickness skin injury (unless complicated by infection) [5], and in contrast to pressure ulcers, lesions develop from the top down, presenting as reddened intact skin, progressing to blistering and loss of epidermal tissue; pressure ulcers develop from the bottom up, progressing toward the surface of the skin [6]. Box 1 outlines the differences between IAD and pressure ulceration [7].
The prevalence of incontinence-associated dermatitis varies between 3.4% and 25%, depending on the care setting and population studied [8].
The following case studies outline how using a skin foam cleanser, in conjunction with a barrier protectant such as Proshield, (H & R Healthcare) helped manage IAD.
Drivers
It had been noted that the tissue viability staff were receiving a number of referrals for help with IAD, and that patients were being poorly managed due to the fact that a variety of products were being used.
As a result, patients were experiencing:
- skin irritation
- erosion of epidermis
- swelling of stratum corneum
- altered lipid rigidity
We therefore wanted to find a product that was clinically effective, cost efficient, easy to use, and that actually worked! We decided to evaluate Proshield Foam & Spray (H & R Healthcare), a pH balanced skin cleanser indicated for both intact and superficially damaged skin associated with incontinence. In addition, it:
- is licensed for use on superficial damage (up to grade 2 Pressure Ulceration)
- is available as a foam and spray no rinse cleanser (solubilisers break down faeces)
- reduces the requirement for multiple products
- maximises time efficiency
- encourages compliance with cleansing regimens
Method
Patients who were to be included in the evaluation gave informed consent for both inclusion into the study and publication of the results (including photographs). Carers participated in the study, and product support was provided by H&R Healthcare.
Patient 1
A 90 year old female living in a nursing home after a cerebro-vascular event (CVE), had a PEG fed. She was doubly incontinent, and had suffered recurring severe excoriation from faecal and urine burns for several months. Prior to inclusion in the study, her skin care regimen comprised of soap and water to cleanse and Cavilon as a barrier cream. (Figures 1 & 2) show the sacral area upon referral and after three weeks cleansing with Proshield.
Patient 2
A 62 year old gentleman with Parkinson's Disease, living in a community hospital; he had a combination of grade 2 pressure damage and moisture damage from urinary incontinence. Treatment comprised soap and water and Canestan cream. He was also on an alternating air mattress and regular turns. After one week, his skin had improved (Figures 3 & 4).
Patient 3
A 65 year old male with Huntington's Disease with some urinary leakage. He initially had grade 2 pressure damage to his sacrum. The staff mistakenly applied the Proshield Skin cleanser and barrier cream to the broken area only; this however, healed within two weeks, but he developed moisture damage to other areas. With re-education to use on vulnerable areas to moisture, the skin was healthy within two further weeks of treatment (Figures 5 & 6).
Evaluation
The product was simple to use. In addition, the following benefits were fed back from the carers.
- no bowls of water at the bedside are required therefore reducing the risk of cross contamination
- no rinsing is required
- it can be used on broken skin
- an improvement in skin condition noted, the majority within a short time-frame, leading to an improvement in quality of life
Conclusion
As a result of the evaluation, we added Proshield to our formulary for patients with grade 6/7 stools (Bristol Stool chart) [9]. We have also included prevention and management of IAD in the PU training day.
It must be recognised this was a very small study and that the positive results may be due to the evaluation encouraging a more rigorous skin hygiene regimen, using a pH balanced product, and achieving continuity of care using one product rather than an array of different products.
With an ever increasing market for skin care products it is essential that nurses keep abreast of what is available, so they can advise patients/carers to make an informed choice. More studies providing robust and rigorous evidence on a large scale are required.
To conclude, good continence care is required in the prevention and management of IAD; this includes identifying individuals at risk of incontinence and ensuring that excessive contact of the skin with moisture is avoided.


























