Exudate: friend or foe?
Sylvie Hampton, RGN, Wound Care Consultant, Eastbourne
Background reading
http://www.woundsinternational.com/media/issues/82/files/content_42.pdf
http://www.woundsinternational.com/media/issues/272/files/content_8812.pdf
What is exudate?
Exudate is fluid that is produced from a wound and can constitute both ‘good news’ and ‘bad news.’ It aids acute wound healing, but can delay healing in chronic wounds.
The concept of moist wound healing has led the way in selection and application of dressings, with the basic concept being that the presence of exudate in a wound will provide an environment that stimulates healing [1] (‘good news’).
However, while moisture is necessary for healing, an overly wet environment may damage both the wound bed and the surrounding skin [2](‘bad news’). It is unclear when its detrimental effects begin to outweigh the benefits [3], therefore, this article will discuss arguments for and against exudate and how any ‘bad news’ might be addressed.
Exudate through time
Humoral theory, also known as humorism, or the theory of the four humours, was a model for the workings of the human body. It was systemised in Ancient Greece, although its origins may go back further still. The theory was central to the teachings of Hippocrates and Galen and it became the dominant theory in Europe for many centuries.
Blood was one such humour; purging with laxatives, blistering the skin with hot irons, and blood-letting were employed to rid the body of any excess of blood, thought to be causing an imbalance of the humours, and thus illness.
As well as the theory of humours, the ancient Greeks believed that suppuration of a wound was an expected feature of its natural history, and the physician encouraged the flow of what the Romans later called ‘pus bonumet laudabile’ (laudable pus). This pus was supposed to facilitate the elimination of unhealthy humours from the injured body, and the idea held sway until the 19th century [4]; indeed, prior to Lister and Pasteur, it was common practice to remove pus from one wound and place it in another…
Unlike the Greeks, we are now fully aware that we cannot transfer bacteria from one person’s wound to another’s and, therefore, we are now very structured around hand hygiene to ensure that transfer does not occur. We are also a great deal more aware of the need to protect the wound and to ensure the wound is not overly moist.
What does exudate do?
Wound exudate fulfils an important function in healing wounds [2],[3] and is believed to have antibacterial properties [5].
During the inflammatory response, blood vessel walls dilate and become more porous allowing protein-rich fluid to filter from the circulatory system into the wounded area [6]. This extracellular fluid formation results in an increased production of exudate [7].
Although wound exudate is necessary for healing, clinicians are now aware that chronic wound exudate is harmful when excessive, contributing to skin maceration and delaying wound healing. This is due in part to the proteolytic enzymes produced in a wound; leukocytes migrate through the wound matrix and release proteases (activated enzymes). These are necessary for:
- the regulation of cell maturation and multiplication
- collagen synthesis and turnover
- the development and removal of the peri-vascular fibrin cuffs found in venous insufficiency and leg ulceration
- the phagocytosis of debris, microbes following inflammation [8]
In a chronic wound, these enzymes can actually delay healing and ‘burn’ surrounding skin (Figure 1).

One of the problems associated with exudate is that no one yet has established the moment that a wound becomes chronic, as each has variables that would delay or speed up healing. The colour of the exudate can be a clue of chronicity; as the wound becomes chronic and takes on more surface bacteria, the exudate begins to change colour and will have a stronger odour. The colour and the odour will indicate the type of bacteria that is present in the wound; green means it is likely to be Pseudomonas, which has a distinct odour, muddy red/brown is possibly Staphylococcus or Streptococcus, with an odour of stale blood.
The presence of these bacteria, the colour and the odour of the wound, does not indicate clinical infection but is most likely represents bacterial colonisation. Colonisation can be managed with dressings, whereas clinical infection (spreading cellulitis, pyrexia, increased odour, pain and exudate) requires antibiotics. Swabs should only be taken if the latter is suspected.
Leg ulceration is unique; due to the underlying condition, hydrostatic pressure in the venous system causes the veins to distend, widening cell junctions and permitting the passage of fluid into the wound surface.
Finding a method of addressing gravity (particularly in dependent legs) is preferable to applying thick absorbent dressings, which do not address the underlying cause. Compression therapy will assist in reversing the pathology that creates the problem [9].
Exudate control
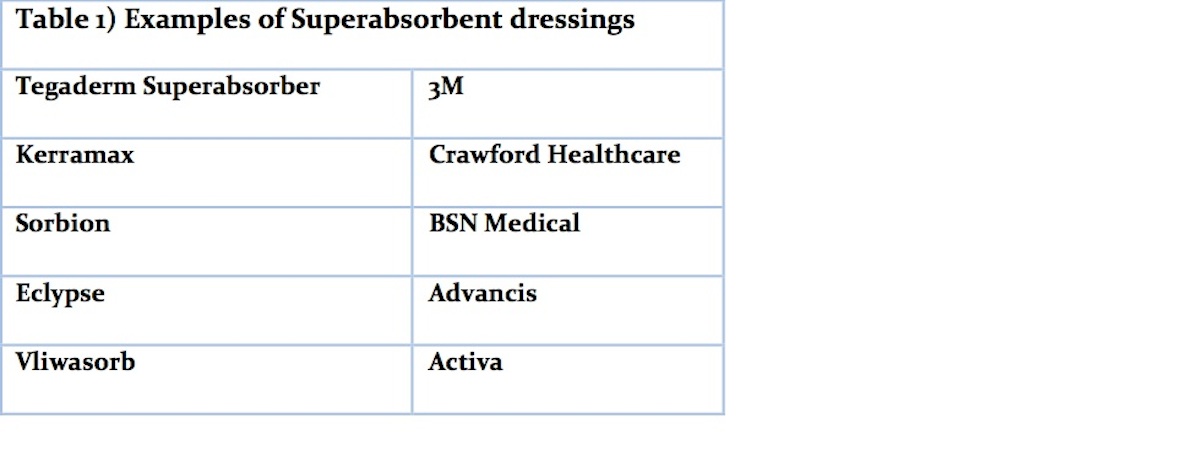
Treating the underlying cause of excessive exudate-generation and selecting appropriate dressings are now the keys to effective management of exudate. Highly absorbent dressings absorb and lock away exudate, reducing its harmful effects. Examples of such dressings are outlined in Table 1.
Honey dressings and iodine dressings are possibly the most cost effective for reducing bacteria. Unfortunately, iodine is negated very quickly in the presence of exudate, so iodine cadexomers, which slowly release iodine into the wound in exchange for wound exudate, are better. Silver is widely used but can be expensive.
As the exudate production reduces through good compression and/or antibacterial dressings, then good foam dressings or advanced fibre dressings are ideal. A wound should never be permitted to remain wet or the surrounding tissues will be macerated and the wound bed will not repair as it should.
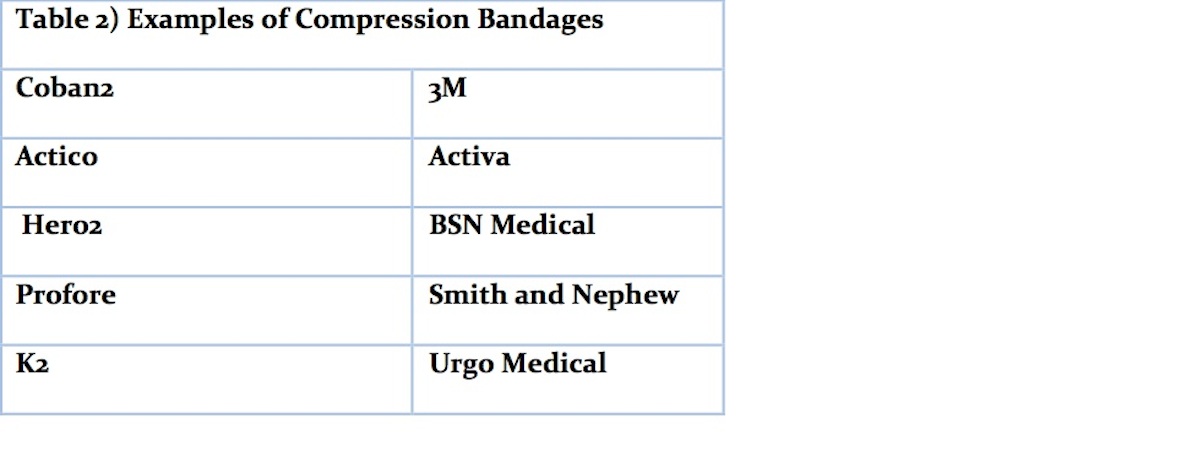
Compression bandages or hosiery should be the first consideration for venous leg ulceration to address the gravity issue. Hosiery can provide the patient with independence as they are able to remove them and apply them, and continue with activities of living. Table 2 provides examples of compression bandages and Table 3, examples of compression hosiery.
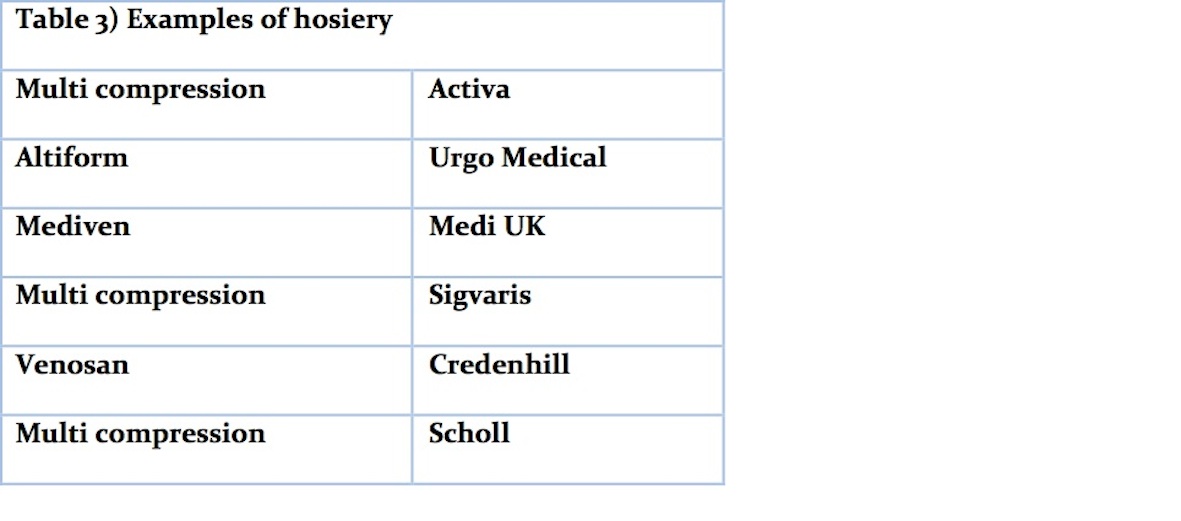
For those patients who do not have the dexterity or the strength required to apply their own hosiery, a product such as Juxta Cures (Figure 2) would be an ideal choice.
These can be applied by anyone with just the simplest of explanation. They are also very cost effective as they can be removed and washed and reapplied for many months.

Conclusion
Exudate is necessary in acute wounds but needs controlling in chronic wounds. Treating the underlying cause of excessive exudate-generation and selecting appropriate dressings are the keys to effective management and by addressing the problem of limb dependency and bacterial colonisation the exudate will reduce.


























