Importance of dressings in exudate control and healing
Sylvie Hampton. MA BSc (Hons) DpSN RGN, Independent Tissue Viability Consultant Nurse
Introduction
Dressings are only a small part of healing and fall behind tackling the cause of a wound and psychosocial issues. They are, nevertheless, a part of healing once the cause of the wound has been addressed. The dressing then increases in importance as careful selection ensures that symptoms are no longer problematical and cost of individual wound care is minimised. When implemented properly, wound management using appropriate interventions based on accurate diagnosis, delivers benefits to patients, healthcare systems and society [1,2].
Chronic wounds are rarely seen in individuals who are otherwise healthy [3], but as the population ages, there will be a greater number of people with comorbidities. At present, 70%-80% of community nursing time is spent on wound management [4] at a cost of £2.03m per 100,000 population, based on 2006-2007 prices [5]. A study in Uppsala, Sweden, showed that in a community of 288,000 people with a typical wound prevalence of 2.4/1000, required the equivalent 57 full-time nurses for dressing changes alone [6] and these numbers will rise as the amount of those who are unwell increases. This is extremely costly.
At this level of obligation, each clinician must have a responsibility to treat wounds appropriately and cost-effectively and, therefore, cost-effectiveness must be a central issue in many wound care decisions. Although clinicians are frequently required to justify clinical decision making in terms of health benefits obtained and the cost to health service providers, few clinicians actually have the skills to accurately interpret cost in more than local health economic terms, and the disjointed structures that exist in healthcare provision mean that even those who monitor health expenditure have little concept of the global cost of care provision [7]. Ignorance of cost can no longer be acceptable.
Wound healing represents the outcome of a large number of interrelated biological events which are orchestrated over a temporal sequence in response to injury and its micro-environment [8,9]. Nevertheless, wounds have only a 10% chance of healing without appropriate intervention [10,11] and if bacteria succeed in forming a biofilm within the wound bed, they will be extremely difficult to eradicate, other than by surgical or mechanical wound debridement [12].
Chronic to acute
Common to all studies of wound healing modalities is the need to convert the chronic wound into an acute wound and to maintain the wound in an acute state [13]. Nevertheless, despite inherent differences in the pathophysiology of acute and chronic wounds, including those in the aged, and variations in their progression, 'healing' or 'complete wound closure' is considered to be the primary outcome measure of both wound types [14]. However, if a wound is treated appropriately and is turned from a sloughy, malodorous wound to one that is granulating, then, in the author’s opinion, the aim has been achieved as a granulating wound is far more likely to achieve closure than one that is not prepared for healing.
Chronic wounds contain a hostile biochemical environment including elevated levels of inflammatory cytokines, free radicals and proteases irrespective of the underlying aetiology[15,16]. Elevated protease activity contributes to intractable wound chronicity [17,18] and 28% of all non-healing chronic wounds have elevated protease activity [10]. Many studies have investigated the role of proteases in human chronic wounds, and have concluded that elevated protease activity contributes to their chronicity [17,18].
Antimicrobial dressings are widely used for management of wound bioburden and are frequently used in combination with other topical therapeutics, such as debridement for the removal of wound necrotic tissues and such combined applications may have greater potential to achieve multiple healing activities simultaneously, including exudate and bioburden management, debridement, and tissue regeneration [19].
Current research is also being targeted at anti-biofilm strategies needed to restore an optimal wound-healing environment and a combined treatment approach involving aggressive debridement and the addition of anti-biofilm agents is needed [20].
Dressings
The overarching goal of wound healing is not necessarily healing itself but the ability to turn a wound from a malodorous, painful and/or sloughy deep wound to one that is clean, with no or little odour and with granulation tissue in the base and dressings are able to assist the clinician in changing the wound environment.
The selected dressing needs to enable a reduction in:
- Pain
- Malodour
- Exudate
- Bacteria
- Devitalised tissue
The dressing needs to provide:
- Warmth
- The optimal balance of moisture in the wound bed
- Absorption of fluid
- Containment or removal of bacteria
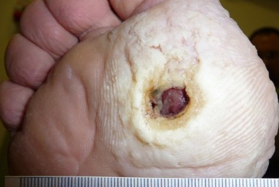
Interventions which can speed the healing rate in individuals with slowly healing or non-healing wounds are of critical importance [21] and the concept of moist wound healing is known to enhance wound healing rates. Moist wound healing has been examined and gradually accepted by wound care clinicians during the last 40 years, and has led to the development of hundreds of dressings that support a moist wound environment [22]. However, the understanding of what is moist and what is wet seems to be missing. A wound should never be kept ‘wet’ or the tissue will become macerated (Figure 1). Therefore, there is a difference between ‘moist’ which is important to healing and ‘wet’ which has adverse affects on healing.
There are numerous specialty dressings available that combine various attributes to enhance wound healing. Dressings are either described as primary, where materials are placed into the wound and interact with the actual wound surface, or secondary where dressings cover and secure the primary dressing in place [23]. Generally, the primary dressing will interact with the wound (honey, silver, PHMB, Iodine, Zorflex, Sorbact etc). The secondary dressing would be an absorbent and retentive dressing such as an adhesive foam. It can be a superabsorbent dressing such as those containing fibres and superabsorbent particles.
Therefore, in a wound that requires cleaning and is malodorous, an interactive dressing, such as honey, PHMB, Iodine cadexomer, Zorflex or Sorbact or silver would be ideal and, if exudate is high, cover with a superabsorbent such as KerraMax, Mextra, Flivasorb, ELECT (these are a few of the superabsorbent dressing types).
A superabsorbent dressing is capable of absorbing high amounts of fluid while keeping the surrounding skin dry (Figure 2). Superabsorbents can cover large areas (Figure 3).
Superabsorbent dressings
The amount of exudate a dressing can hold is also influenced by the way the material handles the fluid [24]. Simple products such as gauze absorb (small amounts) exudate at the point of contact with the fluid while other dressings spread the fluid across the whole of the dressing, giving a greater fluid-handling capacity [24]. Although wound exudate is necessary for healing, experienced clinicians are now aware that chronic wound exudate is harmful to chronic wounds when its production becomes excessive, contributing to skin maceration and delaying wound healing [25]. This is where superabsorbent dressings come ‘into their own’ and are not only cost effective but are clinically effective as well.
Superabsorbent dressings may be used as primary dressings. The action of absorption would ‘pull’ the bacteria into the central core of the dressing, away from the wound. For non-critically colonised wounds, this is an inexpensive and appropriate use of the superabsorbent.
Iodine Dressings
Iodine in the form of Iodoflex or Iodosorb, is auseful dressing agent. Iodine is an antiseptic that bacteria have not yet learned to resist [26,27]. The cadexomer has a broad spectrum antimicrobial action which is delivered by a sustained release of iodine and adesloughing action is provided by the unique cadexomer matrix [28].
Goldheim [29] reports that povidone-iodine is possibly less injurious to wounds than water and would not affect wound healing adversely [29,30].
Honey Dressings
The use of honey as a wound dressing material, an ancient remedy that has been rediscovered, is becoming of increasing interest as more reports of its effectiveness are published. The clinical observations recorded are that infection is rapidly cleared, inflammation, swelling and pain are quickly reduced, odour is reduced, sloughing of necrotic tissue is induced, granulation and epithelialisation are hastened, and healing occurs rapidly with minimal scarring [31].
Silver Dressings
Vermeulen et al. [32] claimed there was insufficient evidence to recommend the use of silver-containing dressings or topical agents for treatment of infected or contaminated chronic wounds and yet Beam [33], found exactly the opposite inthat use of silver foam dressings resulted in a greater reduction in wound size and more effective control of leakage and odour than did use of non-silver dressings.
Based on the vast majority of in vivo studies available, silver does not adversely effect viable cells and, thus, is not cytototoxic [34].
Zorflex
Long fibre activated carbon (Zorflex) has been used in wound care for many years. The material is used in armed forces uniforms as protection against bacterial and chemical warfare. It is a natural step to use this same protection in wound care. Recently, in vitro tests, undertaken by UK Health Protection Agency, demonstrated that long fibre activated carbon, used in uniforms and in dressings, was both antiviral and virucidal, with virus kill rates of up to 98% [35].
Zorflex has been shown in pilot studies to demonstrate strong ability to lessen and change the bacterial loading, reduce associated pain and malodour, and effectively ‘clean’ the wound bed to allow healing to occur over seven to 14 days of use [36].
Sorbact
Sorbact uses sterile hydrophobic acetate or cotton fabric, plus the absorption dressing has an absorption core of non-woven viscose which is thought to rival silver in its ability to reduce the overall concentration of microbes in a wound each time the dressing is changed. When in physical contact with the wound bed, and in the presence of moisture, bacteria are attracted to the dressings and become irreversibly bound to it. This reduces the overall concentration of microbes in the wound and this process is called hydrophobic interaction.
Conclusion
Managing potentially highly exuding wounds can be complex with multiple factors and there is a need for constant vigilance and reassessment of patients. For wounds that have strong malodour and are likely to be critically colonised, then an antibacterial dressing is required with a superabsorbent secondary dressing. For wounds that are minimally colonised but with high exudate, then a superabsorbent dressing would be the answer.