RAY NORRIS, RGN, Clinical Nurse Specialist Tissue Viability, South West Essex Community Services, North East London NHS Foundation Trust, Brentwood Community Hospital
A substantial increase in the number of residential home patients referred to the Integrated Community Team (ICT) for pressure ulcer management highlighted the need for ongoing improvements in care standards with these homes. In response, a project was defined with the specific aim of enhancing the standard of care within RHs. This article, adapted from a poster presented at the European Wound Management conference 2014, outlines a collaborative initiative between the Tissue Viability Service, Basildon ICT, and Smith & Nephew.
Aim
The aim of the project was to improve the quality of care and thereby reduce pressure ulcer (PU) incidence within a group of eight residential homes (RHs) in South West Essex. The project intervention comprised:
- the implementation of SSKIN Bundle education
- targeted use of Aderma dermal pads and Proshield to aid pressure ulcer development
Method
For three months prior to the start of the study, PU incidence data was collected from each of the NHs involved in the project. The same data were collected in all homes over the three month period immediately after initiation of the project. The impact achieved by the project was measure by a comparison of these two sets of data.
Pressure ulcers are considered a nurse-sensitive indicator of quality as the development of pressure damage is often multifactorial and related to the breakdown of individual elements of nursing care [1]. The NHS East of England and Midlands SSKIN Bundle [2] (Figure 1) was chosen as the educational tool, and an action plan was developed within the homes to address other issues which could also be related to the SSKIN Bundle.
ADERMA dermal gel pads redistribute pressure to protect bony areas from skin damage caused by pressure, most notably the heel and sacrum. They can be washed and re-used by the same patient, so are cost-effective. Studies have demonstrated that ADERMA contributed to a 75% drop in the number of pressure ulcers in an acute trust across four wards [3] and across three nursing homes, and showed a visual and below-the-skin improvement when used on category I pressure ulcers, all of which healed within weeks of commencing treatment [4].
Preparatory meetings were held between the Integrated Community Team (ICT), Smith & Nephew, and the Tissue Viability (TV) team to establish role boundaries and agree actions for the project delivery. The TV team supervised the project and supported the ICT with the implementation and on-going local support. Smith & Nephew delivered an educational package which focused on the SSKIN Bundle, and provided training on the appropriate use of ADERMA dermal pads for the care staff in each of the RHs. A ‘stock box’ was issued to each RH immediately after training; this contained initial supplies of ADERMA dermal pads for staff to use where risk assessment identified the need for immediate off-loading. During this process, the ICT developed relationships with management and carers at the RHs and introduced the concept of working together utilising evidence based tools to improve quality of care. Following the educational sessions, all residents were assessed by the ICT for pressure ulcer development risk, and an individualised care plan for prevention developed. The SSKIN Bundle was then completed by the care staff on each shift and reviewed by the ICT staff where necessary or any if deterioration were noted, or concerns were raised by the staff.
Results
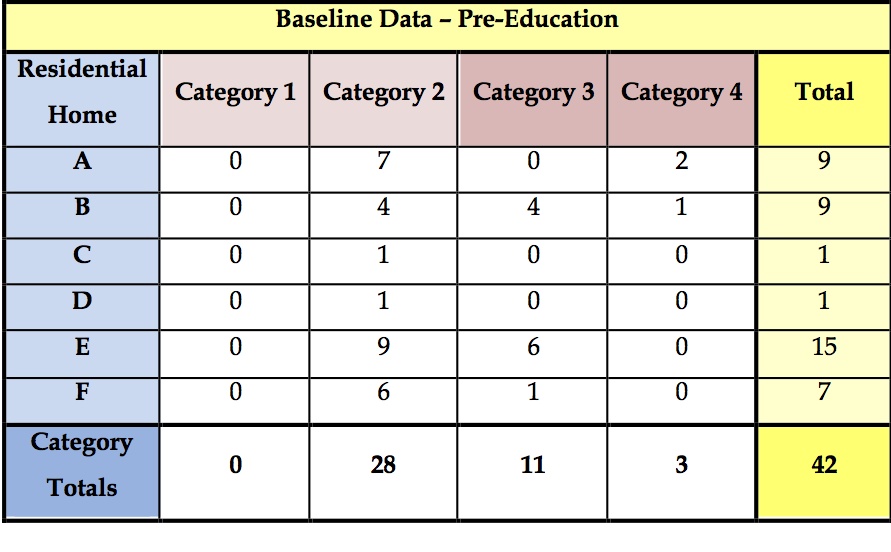
Across the six RHs, a total of 42 PU were recorded in the course of the 3-month baseline data collection period (pre-study) (Table 1). All were deemed avoidable at the time as no documentation was evident.
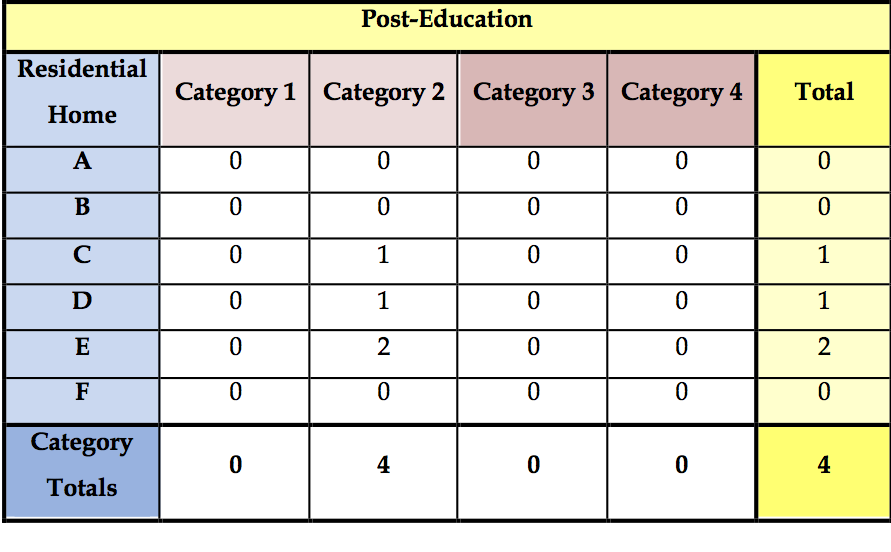
In the 3-month comparator period following the educational initiative, only four PUs were recorded, all of which were Category 2 and classified as unavoidable as all relevant documentation and assessments were complete (Table 2). The number of referrals to the ICT for skin tears / traumatic wounds decreased and residents were seen by ICT staff weekly when the SSKIN Bundle and care plans were reviewed.
Anecdotal feedback from the Safeguarding Team complimented the reduction in safeguarding concerns and the increase in quality of care. One homes’ recent Care Quality Commission (CQC) inspection noted the positive influence that the project has had within the home, and that this was an example of good practice. The home has adopted the use of the Pressure Ulcer Safety Cross, and the staff feel confident to display this as an indicator of the quality of care they provide to residents. Indeed, despite an outbreak of diarrhoea and vomiting within the home, no pressure ulcers or moisture lesions developed, again highlighting the increase in quality of care.
Discussion
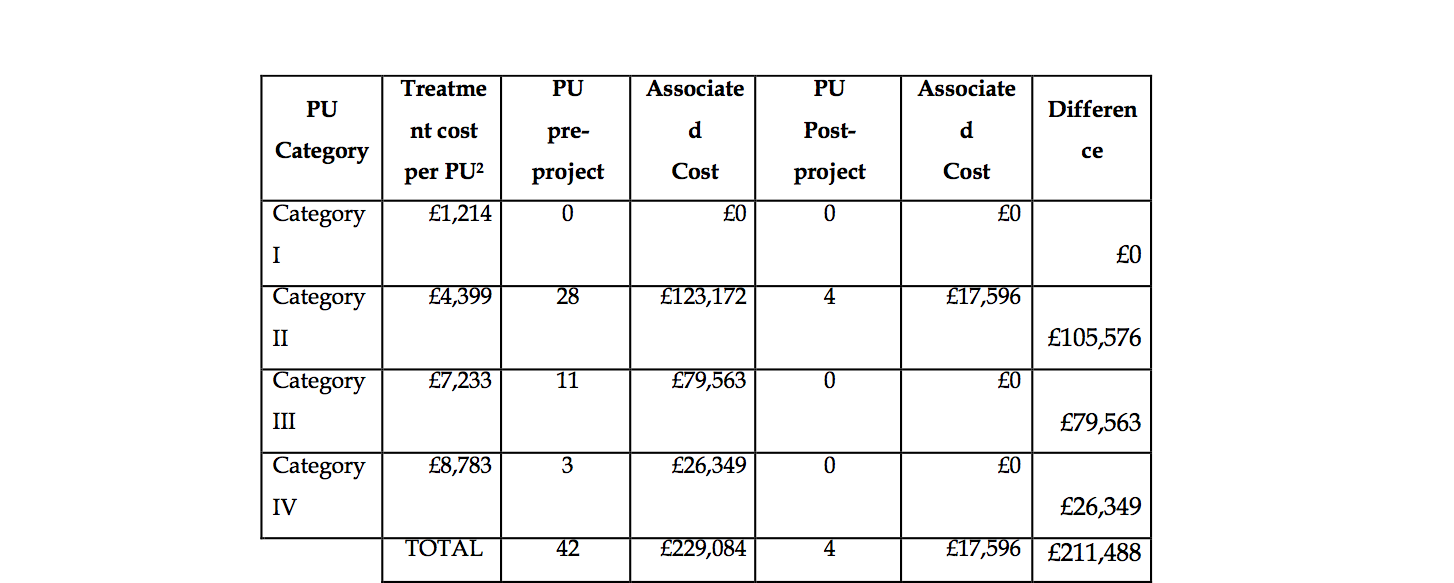
A simple analysis was performed in which published reference costs for the PU management were applied to the numbers of PU recorded pre- and post- educational initiative [5].
The analysis (Table 3) indicates that the reduction in PU incidence following the educational initiative is associated with a saving of over £200,000 compared to the costs associated with the treatment of the number of PU recorded prior to the initiative.
Key project outcomes:
- A reduction in PU development was recorded following SSKIN Bundle education and the introduction of targeted use of ADERMA dermal pads
- Carers identified a delay between District Nurse referral and the provision of off-loading devices. During this interval PUs did develop in some cases. This observation emphasises the vital role fulfilled by the supply of ‘stock boxes’ which enable staff to address PU risk immediately without any delay
- The ongoing impact of the project will be monitored as Statistical Process Control chart against PU dashboard in relation to development of Category 2 PUs
- On the basis of this project the CCG has confirmed funding for the wider roll out of the project approach as a two year initiative within nursing homes to achieve zero tolerance
The cost saving to the nursing homes will of course be less than this figure as this represents a health economy-wide saving including such costs as hospitalisation, etc. In addition, none of the cost associated with the initiative have been considered (for example, increased use of preventative products such as Aderma). Even so, the cost savings associated with this preventative approach would be sizeable since the material cost of items such as Aderma are relatively low compared to the cost of managing a PU.
During the implementation of the project, much was learnt about joint working across specialities and the differing levels of knowledge amongst staff, which created a common level of delivery. Despite the initial increase in workload, the enthusiasm and commitment of the ICT staff responsible for the residential home was a critical success factor in the pilot. The willingness of management and care staff at the residential home also contributed significantly to the project’s success.
Conclusions
The results of this project have been incredibly positive and demonstrate a model that strives to achieve the ‘zero tolerance’ initiative of avoidable PUs. It should be repeatable elsewhere. The structured approach of combining the SSKIN Bundle and ADERMA training ensured all staff used ADERMA appropriately as a way of reducing the risk of pressure damage. The project illustrates that although pressure ulceration was the initial focus, other secondary outcomes were also achieved and reflected in the improved quality of care.
This project illustrates how a structured collaborative working approach between care providers and the healthcare industry can be highly effective. This project is an example of how industry can help support clinicians in meeting the challenge of reducing pressure ulcer occurrence and ultimately improve the quality of care for patients. Due to the success of the project, the same approach will be replicated across the organisation in other residential homes to support improved quality care and the prevention of pressure ulcers.
The success of the project has been communicated across the trust and has promoted much discussion about preventing pressure ulcers and improving care standards. Standards have remained high and the relationship between the community nurses and residential home staff has developed into one of sharing care for patients.


























